HOLISTIC STROKE SOLUTIONS Episode 3: Obvious and Hidden Balance Problems After Stroke
Jun 15, 2025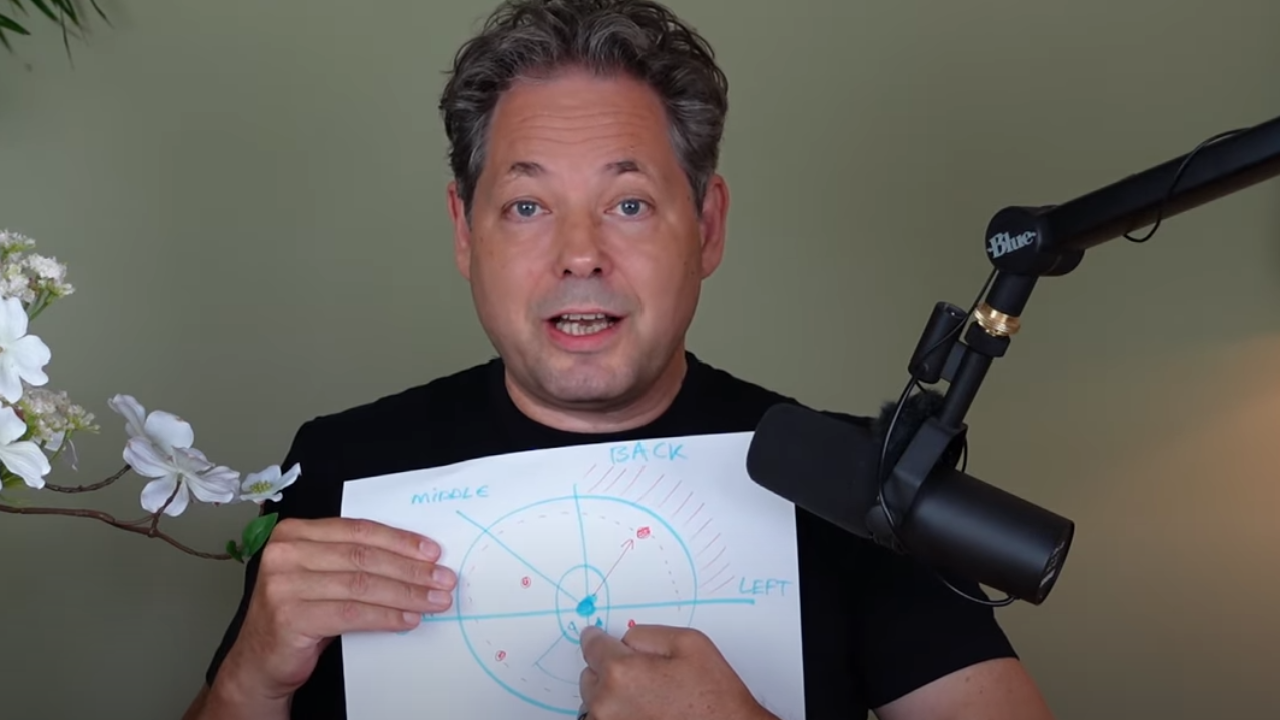
Why You Feel Unsteady After Stroke: The Hidden Balance Problem No One Talks About
Understanding center of pressure changes and what they mean for your recovery
Introduction
If you're a stroke survivor, you've probably noticed that balance feels different now. Maybe you feel unsteady when standing, worry about falling, or find yourself leaning heavily on one side. You're not imagining it, and you're definitely not alone. What you're experiencing has a name - center of pressure changes - and understanding this hidden problem could be the key to better balance and confidence in your recovery.
Your center of pressure is simply where your weight sits when you're standing or moving. After a stroke, this changes dramatically, and current rehabilitation programs often miss this crucial piece of the puzzle. Let's explore why this happens and what you can do about it.
Why Your Balance Changed After Stroke
It's Not Just About Strength
Most people think balance problems after stroke are just about muscle weakness. The truth is more complex and actually more hopeful. Your brain controls balance through several interconnected systems, and stroke affects these in ways that go far beyond muscle strength.
The brainstem connection: Research shows that your brainstem - the part of your brain that controls basic functions like breathing and balance - is actually the strongest predictor of balance problems after stroke. This challenges the common focus on just strengthening muscles.
Both sides of your brain are affected: Even if your stroke only damaged one side of your brain, both sides can be affected when it comes to balance. This explains why even "mild" strokes can cause significant balance issues.
Your body's GPS system is disrupted: Nearly half of all stroke survivors (46.7%) experience problems with something called "body schema" - your brain's internal map of where your body parts are in space. Imagine trying to navigate with a broken GPS - that's what your brain is dealing with when trying to control balance.
The Spatial Awareness Connection
Here's something that might surprise you: where you are in space matters more for recovery than how strong you are. Two important studies found that:
- Motor strength wasn't a significant predictor of how well people recovered after stroke
- Spatial problems (like not being aware of one side of your body) predicted 72% of functional recovery outcomes
- Problems with spatial awareness predicted community mobility at 6 months better than traditional strength measures
This means that even if you get stronger, if your brain can't accurately sense where your body is in space, you'll still struggle with functional activities.
The Direct Path to Falls
The Numbers Don't Lie
Falls are unfortunately common after stroke, with 23-73% of stroke survivors falling within their first year. But here's what's important: specific balance patterns can predict who is most at risk.
Weight distribution matters: Most stroke survivors put about 60% of their weight on their unaffected leg. When this asymmetry is greater than 27%, fall risk increases significantly.
Movement patterns are telling: People who fall show much faster and more erratic balance movements - about 2.7 times greater than healthy young adults.
Technology can predict falls: Researchers can now predict falls with 91% accuracy using balance measurements, showing just how closely connected these balance changes are to actual fall risk.
The Confidence Connection
Balance problems create a vicious cycle. When your balance feels unstable, you naturally become less confident about moving. This leads to moving less, which makes you weaker and more unsteady, which reduces confidence even more. Breaking this cycle is crucial for recovery.
Why Current Rehabilitation Might Be Missing the Mark
The Problem with Generic Exercises
Most rehabilitation programs use generic balance exercises that don't specifically target the center of pressure changes that happen after stroke. While these exercises might help initially, they can actually teach your brain to use compensatory strategies that limit long-term recovery.
The compensation trap: When exercises don't address the root spatial-awareness problems, your brain learns to compensate by relying more heavily on your unaffected side. While this might help you function in the short term, it can actually make recovery harder in the long run.
The research-practice gap: There's a 17-year gap between what research shows works and what actually gets used in clinics. Many effective approaches simply aren't being implemented yet.
What's Missing
Current rehabilitation often misses the connection between spatial awareness and movement. It's like trying to teach someone to drive while they're wearing glasses with the wrong prescription - you can practice all you want, but until you fix the underlying vision problem, progress will be limited.
The New Approach: Technology-Enhanced, Targeted Training
What's Possible Now
Exciting new approaches are showing much better results by specifically targeting the balance and spatial awareness problems that happen after stroke:
Real-time feedback systems: Using force plates and computer feedback, you can actually see your balance in real-time and learn to control it more effectively. One study showed significant improvements in balance scores after using this type of training.
Virtual reality training: VR systems that challenge your balance in safe, controlled environments show superior results compared to traditional exercises, with significant improvements in balance confidence and actual balance performance.
Exoskeleton-assisted training: For those with more severe impairments, robotic assistance can help retrain proper movement patterns. One study showed balance scores improving from about 10 to 32 points in the exoskeleton group, compared to 10 to 20 points in traditional therapy.
Spatial retraining: Specific exercises that retrain your brain's spatial awareness, like prism adaptation therapy, can produce immediate improvements in movement control.
What This Means for You
These approaches work because they address the root cause - the disrupted connection between spatial awareness and movement control. Instead of just trying to compensate around the problem, they actually help retrain your brain's ability to sense where your body is and control movement accordingly.
Practical Steps You Can Take
Advocate for Better Assessment
Ask your healthcare team about:
- Center of pressure measurements
- Balance assessment with dual tasks (like balancing while doing a mental task)
- Spatial awareness testing
- Technology-enhanced balance training options
Look for These Features in Your Therapy
The most effective balance training programs should include:
- Real-time feedback about your balance
- Progressive challenges that gradually increase difficulty
- Tasks that combine balance with cognitive challenges
- Training that addresses both obvious and hidden balance problems
Home Strategies
While waiting for better rehabilitation options:
- Practice balance activities with visual feedback (like standing in front of a mirror)
- Work on spatial awareness through activities that require precise positioning
- Challenge your balance in safe, controlled ways with proper supervision
- Don't avoid movement - work with your therapy team to find safe ways to stay active
Looking Forward: Hope for Better Recovery
The Future is Bright
Research is rapidly advancing in this area. Artificial intelligence is being used to personalize treatment plans, new technologies are making effective treatments more accessible, and our understanding of how the brain recovers after stroke continues to improve.
Precision Rehabilitation
We're moving toward an era of precision rehabilitation, where treatments are tailored to your specific type of balance problems and recovery patterns. This means more effective, efficient rehabilitation that addresses your individual needs.
Conclusion
Balance problems after stroke are real, common, and complex - but they're not insurmountable. Understanding that your balance challenges stem from changes in how your brain processes spatial information and controls your center of pressure is the first step toward more effective treatment.
The key insights to remember:
- Balance problems after stroke are about more than just strength
- Spatial awareness is often more important for recovery than motor strength
- Current rehabilitation approaches may be missing crucial elements
- New technology-enhanced approaches show much better results
- You can advocate for better assessment and treatment
Don't accept that balance problems are just something you have to live with after stroke. The research is clear that targeted, technology-enhanced approaches can make a real difference. Work with your healthcare team to explore these options and advocate for rehabilitation that addresses the root causes of your balance challenges.
Your recovery journey is unique, but you don't have to navigate it without the right tools and understanding. Better balance and greater confidence are possible with the right approach.
References
- Batchelor, F. A., et al. (2012). Falls after stroke. International Journal of Stroke, 7(6), 482-490.
- Barrett, A. M., & Muzaffar, T. (2014). Spatial cognitive rehabilitation and motor recovery after stroke. Current Opinion in Neurology, 27(6), 653-658.
- Genthon, N., et al. (2008). Contribution of each lower limb to upright standing in stroke patients. Stroke, 39(6), 1793-1799.
- Giaquinto, S., et al. (2001). EEG recordings in the course of recovery from stroke. Stroke, 32(11), 2295-2302.
- Hu, X., et al. (2021). Analysis of center of pressure signals by using decision tree and empirical mode decomposition to predict falls among older adults. Journal of Biomedical Informatics, 103, 103381.
- Laver, K. E., et al. (2017). Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews, 11, CD008349.
- Melzer, I., et al. (2004). Postural stability in the elderly: A comparison between fallers and non-fallers. Age and Ageing, 33(6), 602-607.
- Oh-Park, M., et al. (2014). Severity of spatial neglect during acute inpatient rehabilitation predicts community mobility after stroke. PM&R, 6(8), 716-722.
- Semrau, J. A., et al. (2018). Examining differences in patterns of sensory and motor recovery after stroke with robotics. Stroke, 49(2), 405-411.
- Zheng, Q. X., et al. (2024). Exoskeleton rehabilitation robot training for balance and lower limb function in sub-acute stroke patients. Journal of NeuroEngineering and Rehabilitation, 21, 90.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
